HEALTH
Why Nurse Practitioners Need Comprehensive Risk Management Strategies

Nurse Practitioners (NPs) are redefining the landscape of healthcare, filling crucial gaps in access and providing care in underserved areas. As their roles expand into high-stakes environments like emergency care, surgical assistance, and telemedicine, the complexity of their responsibilities increases exponentially. This evolution exposes NPs to heightened risks, from clinical errors to legal liabilities, underscoring the need for robust risk management strategies.
Understanding these risks begins with recognizing the nuances of patient interactions. From prescribing medications to making diagnostic decisions, NPs must navigate a labyrinth of protocols and expectations. Minor oversights can lead to significant repercussions, both for patient health and professional standing. Risk management, therefore, becomes not just a defensive strategy but a proactive one to ensure excellence in care.
Beyond clinical settings, administrative and legal obligations pose additional challenges. Documentation errors, regulatory violations, and inadequate insurance coverage can entangle NPs in disputes, draining time and resources. Comprehensive risk management helps practitioners anticipate these issues, mitigating potential damage before it occurs and enabling them to focus on their core mission—delivering patient care.
Identifying Common Risks in NP Practice
One of the most pressing concerns for nurse practitioners is the potential for malpractice claims. Misdiagnoses, medication errors, and procedural mishaps remain leading causes of lawsuits against NPs. While these risks are not unique to nurse practitioners, their expanding responsibilities make them increasingly vulnerable, especially in high-pressure settings like primary care or specialized clinics.
Another significant area of risk stems from regulatory compliance. Nurse practitioners must adhere to a web of state-specific regulations regarding scope of practice, physician collaboration, and patient privacy laws. Failure to comply with these laws can lead to legal actions, license revocation, or financial penalties. Staying informed and up-to-date on evolving legislation is a cornerstone of effective risk management.
Lastly, operational risks such as burnout, insufficient staffing, and inadequate training can compromise patient care and safety. Nurse practitioners are often at the frontlines, managing heavy workloads and complex cases. Institutions must prioritize organizational support and professional development to mitigate these challenges, ensuring a safer and more sustainable work environment for NPs.
The Legal Landscape: Navigating State and Federal Requirements
State and federal laws present another layer of complexity for nurse practitioners. Each state governs the scope of NP practice differently, from full-practice authority to restrictive collaborative agreements with physicians. Navigating these regulations is a critical component of risk management, as non-compliance can jeopardize an NP’s career.
Federal laws, such as the Health Insurance Portability and Accountability Act (HIPAA), further complicate the legal landscape. HIPAA violations, whether intentional or accidental, can result in severe penalties, including fines and lawsuits. For nurse practitioners operating in telemedicine or using electronic health records, the risk of data breaches adds a modern dimension to their responsibilities.
The Financial Implications of Inadequate Risk Management
Risk management is not just about preventing lawsuits; it’s also about safeguarding financial stability. Malpractice claims can result in devastating financial consequences for NPs, with settlements and legal fees often exceeding personal or employer coverage limits. Inadequate preparation in this area can leave practitioners exposed to life-altering liabilities.
Insurance coverage, particularly malpractice insurance, is a critical aspect of financial risk management. Selecting the right policy requires careful consideration of coverage limits, exclusions, and cost. As discussed in this comprehensive guide, tailored policies provide a safeguard against unexpected claims. Nurse practitioners must evaluate their specific needs and risks, ensuring that their coverage aligns with their practice scope.
Moreover, beyond malpractice, NPs must consider broader financial risks such as billing errors, coding mistakes, and regulatory fines. Establishing a systematic approach to audits, training, and compliance can prevent costly oversights. These steps not only protect financial health but also enhance the operational integrity of NP practices.
Leveraging Technology for Risk Mitigation
In an increasingly digital world, technology offers nurse practitioners new tools for mitigating risk. Electronic Health Records (EHRs) reduce the likelihood of documentation errors while improving continuity of care. Automated systems streamline medication prescribing, flagging potential interactions and dosages before errors occur. These advancements help ensure safer and more efficient practices.
Telemedicine platforms, another technological innovation, enable NPs to expand their reach while minimizing certain risks. However, this medium introduces its own challenges, such as cybersecurity threats and licensing complications. To mitigate these risks, nurse practitioners must implement secure, compliant systems and remain vigilant against emerging threats.
Education and training in technology are paramount. Familiarity with tools like EHRs, risk assessment software, and telehealth platforms allows NPs to use these resources effectively. By integrating technology into their risk management strategies, nurse practitioners can enhance patient safety, improve outcomes, and reduce their exposure to liabilities.
Building a Culture of Proactive Risk Management
Effective risk management is not a solo endeavor; it requires a collaborative culture across healthcare teams. Nurse practitioners should actively participate in organizational risk assessments, quality improvement initiatives, and continuing education programs. A proactive approach empowers practitioners to anticipate challenges rather than merely react to them.
Mentorship and peer support also play vital roles. Experienced NPs can guide newer practitioners through the intricacies of risk management, offering insights based on real-world experiences. Collaboration with other healthcare providers ensures a well-rounded approach to patient safety, reducing the likelihood of oversights.
Ultimately, a culture of risk management fosters resilience and professional growth. By embracing comprehensive strategies—spanning legal, financial, and technological dimensions—nurse practitioners can navigate the complexities of modern healthcare with confidence, protecting themselves and their patients while advancing their careers.
Finally, comprehensive risk management is an indispensable aspect of modern nurse practitioner practice, safeguarding both patient safety and professional integrity. As NPs continue to take on broader responsibilities in diverse healthcare settings, adopting proactive strategies to mitigate legal, financial, and operational risks is critical. By leveraging tools like tailored insurance coverage, technological advancements, and collaborative support systems, nurse practitioners can navigate the complexities of their roles with confidence and focus on delivering high-quality care. Ultimately, a commitment to thorough risk management not only protects practitioners but also enhances the overall standard of healthcare.
HEALTH
Attrities: Causes, Symptoms, and Ways to Improve Quality of Life
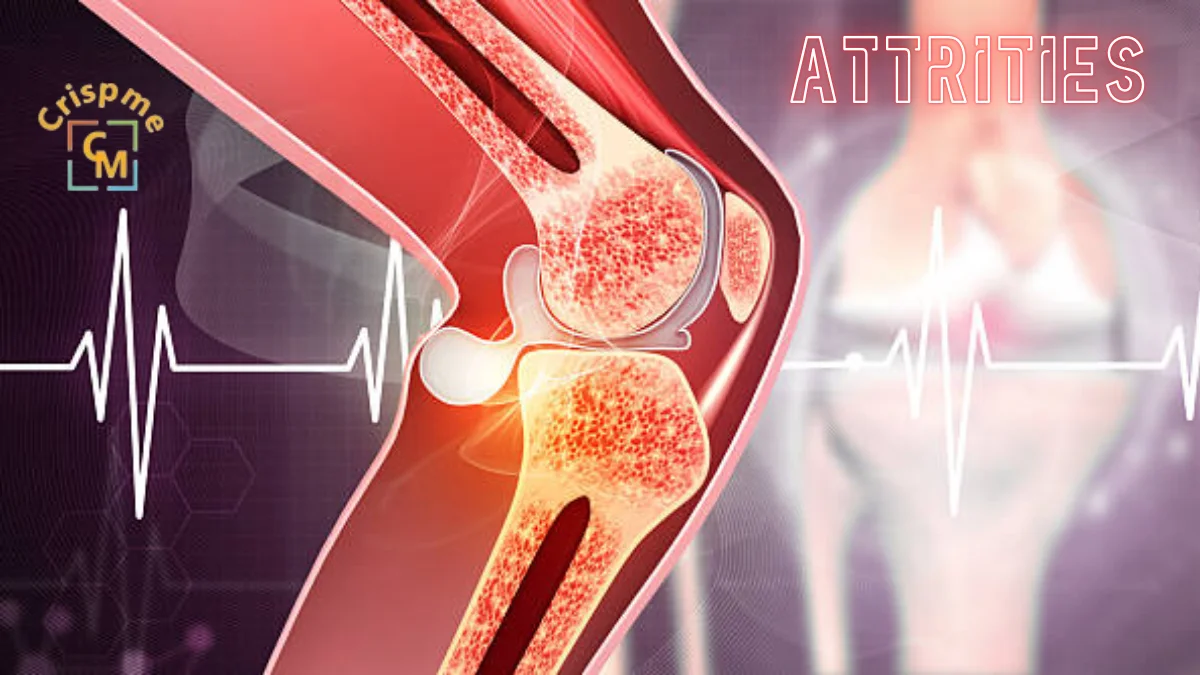
Attrities is a term that often surfaces in conversations about joint pain, but its impact goes far beyond mere discomfort. For millions of people, attrities can encroach on daily activities and affect quality of life. Understanding this condition is vital for anyone navigating its challenges or supporting someone who does.
With various types presenting unique hurdles, it’s crucial to recognize the symptoms early and seek appropriate treatment. From lifestyle changes to exercises tailored for relief, there are numerous ways to manage attrities effectively. This blog post will explore the intricacies of attrities: its causes and symptoms, diagnosis options, effective treatments, and supportive therapies designed to enhance well-being.
Whether you’re newly diagnosed or have been living with attrities for years, understanding your path forward can empower you in managing this condition successfully. Let’s delve into what you need to know about living well with arthritis.
Understanding Attrities
Attrities is a complex condition that primarily affects the joints, causing inflammation and pain. It can occur in various forms, each with its own characteristics and triggers.
At its core, attrities results from the immune system mistakenly attacking healthy joint tissues or wear and tear over time. This leads to swelling, stiffness, and often significant discomfort.
The prevalence of attrities is staggering; it affects people of all ages, genders, and backgrounds. Understanding this condition begins with recognizing that it’s not just an “older person’s disease.”
Genetics, lifestyle factors like diet and exercise habits, as well as environmental influences can all contribute to developing attrities. Knowing these details helps demystify the challenges faced by those living with this chronic illness.
Types of Attrities and their Causes
Attrities is not just one condition; it encompasses over 100 types. Every form presents distinct causes and features.
Osteoattrities, the most common form, often results from wear and tear on joints over time. Aging plays a significant role here. Joint injuries can also lead to this degenerative condition.
Rheumatoid attrities is an autoimmune condition in which the immune system wrongly targets the joints. Genetics and environmental factors contribute to its onset.
Psoriatic attrities occurs in some individuals with psoriasis, linking skin issues with joint inflammation. The exact cause remains elusive but may involve genetic predisposition.
Gout arises from excess uric acid in the bloodstream, leading to sudden, severe pain usually in the big toe. Dietary choices can influence these levels significantly.
Understanding these different types helps tailor appropriate treatment strategies for those affected by attrities.
Common Symptoms of Attrities
Attrities presents a range of symptoms that can vary from person to person. Joint pain is the most common complaint, often described as a dull ache or sharp sensation during movement.
Swelling around affected joints may also occur. This inflammation can lead to stiffness, making it difficult for individuals to perform everyday tasks.
Another notable symptom is fatigue. Many people with attrities experience tiredness that seems unrelated to their activity level. This overall exhaustion can impact daily life significantly.
Additionally, some might notice changes in joint appearance. Deformities or nodules may develop over time, signaling progression of the condition.
Reduced flexibility is a frequent issue associated with attrities. People often find they cannot bend or stretch their joints fully without discomfort, limiting mobility and independence in activities.
Diagnosis and Treatment Options
Diagnosing attrities involves a thorough examination of your medical history and physical condition. Healthcare providers often perform blood tests and imaging studies, such as X-rays or MRIs, to determine the type and severity of the disease.
Once diagnosed, treatment options vary widely based on the specific type of attrities you have. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce pain and inflammation. For some patients, corticosteroids may be recommended to suppress immune responses.
Disease-modifying antirheumatic drugs (DMARDs) can help slow disease progression in inflammatory types like rheumatoid attrities. Physical therapy is also beneficial for improving joint function.
In serious cases, surgery may be required to restore or replace affected joints. It’s crucial to work closely with healthcare professionals to tailor treatments that suit individual needs for optimal management of attrities symptoms.
Lifestyle Changes to Improve Quality of Life
Making small lifestyle changes can have a significant impact on your quality of life when dealing with attrities. Start by focusing on nutrition. A balanced diet rich in antioxidants, omega-3 fatty acids, and whole grains can help reduce inflammation.
Staying hydrated is equally important. Water aids joint lubrication and overall bodily functions. Aim to drink enough water daily to keep your body functioning optimally.
Sleep also plays a crucial role in managing attrities symptoms. Establishing a consistent sleep routine enhances rejuvenation and reduces fatigue.
Incorporating stress-reduction techniques like meditation or yoga can improve mental well-being too. These practices not only calm the mind but may also alleviate physical tension caused by stress.
Setting realistic goals for activity levels encourages movement without overwhelming yourself. Gentle activities promote mobility while respecting your body’s limits, empowering you to take control of your journey with attrities.
Exercises for Attrities Relief
Exercise plays a vital role in managing attrities symptoms. It helps to maintain mobility and reduce stiffness. Even gentle movements can make a significant difference.
Low-impact activities are ideal for those dealing with attrities. Swimming and cycling provide excellent cardiovascular benefits without putting pressure on the joints. These exercises keep the body active while minimizing discomfort.
Stretching is essential too. Simple stretches can enhance flexibility and range of motion, making daily tasks easier. Consider incorporating yoga or tai chi into your routine; they promote balance alongside relaxation.
Strength training should not be overlooked either. Building muscle around affected joints provides extra support, which may help alleviate pain over time. Using resistance bands or light weights is an effective way to start safely.
Always consult with a healthcare professional before beginning any new exercise program tailored specifically for your needs and abilities will yield the best results in your journey toward better health.
Alternative Therapies for Managing Attrities Pain
Alternative therapies can offer relief for those managing attrities pain. Many individuals find comfort in practices like acupuncture, which involves inserting thin needles at specific points on the body to promote healing and reduce discomfort.
Herbal remedies are another popular option. Turmeric contains curcumin, a compound known for its anti-inflammatory effects. Incorporating it into your diet may help alleviate symptoms.
Practices that connect mind and body, like yoga and meditation, may also offer benefits. These practices not only improve flexibility but also foster relaxation, helping to combat stress that often exacerbates pain.
Essential oils like peppermint or lavender may provide soothing effects when used in massages or diffusers. The aroma can create a calming environment while potentially easing muscle tension.
Before trying any alternative therapy, consulting with a healthcare professional is wise to ensure safety and compatibility with existing treatments.
Coping with Emotional Effects of Attrities
Living with attrities can take a toll on emotional well-being. Chronic pain and fatigue often lead to feelings of frustration and sadness.
It’s essential to acknowledge these emotions. You’re not alone in what you feel. Many people experience similar challenges, which can help create a sense of connection.
Finding healthy coping mechanisms is crucial. Consider journaling your thoughts or engaging in creative activities like painting or knitting. These outlets can provide relief and distraction from daily discomforts.
Mindfulness practices, such as yoga or meditation, may also be beneficial. They encourage relaxation and foster a positive mindset.
Talking to friends, family, or support groups about your experiences can ease the burden too. Sharing your story creates understanding and allows for mutual support during tough times.
Remember that seeking professional help is always an option if feelings become overwhelming. Mental health matters just as much as physical health when managing attritieseffectively.
Support Systems for Attrities Patients
Support systems play a crucial role in managing attrities. They provide emotional strength and practical assistance when needed most.
Family and friends can be invaluable resources. Their understanding and encouragement help ease feelings of isolation often experienced by those living with chronic pain. Simple gestures, like cooking a meal or offering to run errands, make a significant impact.
Joining support groups is another excellent way to connect with others facing similar challenges. Sharing experiences fosters camaraderie and provides insights into coping strategies that work for different individuals.
Online forums also offer valuable connections without geographical limitations. Patients can seek advice, share stories, and even find motivation through digital communities.
Healthcare professionals should not be overlooked as part of the support system. Regular check-ins with doctors or physical therapists ensure tailored care while addressing concerns about medication or exercise routines effectively.
Conclusion
Attrities is a multifaceted disorder impacting millions of individuals around the globe. It’s not just an old person’s ailment; it can strike at any age and significantly impact daily life. Understanding the various types of arthritis, their causes, and symptoms is crucial for effective management.
Treatment options vary widely from medications to physical therapies. Each individual’s needs are unique, so personalized care plans are essential for improving quality of life. Lifestyle changes like diet modifications and regular exercise play a significant role in managing attrities symptoms.
For those seeking relief beyond traditional methods, alternative therapies such as acupuncture or massage can offer additional support. Emotional well-being should also be a priority; it’s important to acknowledge the psychological toll attrities can take on individuals and their families.
Fostering connections with support groups or communities dedicated to attrities can provide invaluable encouragement and advice through shared experiences. Embracing these strategies will help many navigate the challenges posed by this chronic condition more effectively while enhancing overall well-being.
HEALTH
GyneCube: Silicone Support for Women’s Wellness

Introduction to GyneCube
In a world where women are constantly juggling responsibilities, self-care often takes a backseat. Yet, prioritizing wellness is essential for every woman. Enter GyneCube a revolutionary silicone support designed specifically with women’s health in mind. This innovative product aims to empower women by addressing their unique needs and challenges. Whether you’re seeking relief from discomfort or simply aiming to enhance your overall well-being, GyneCube might just be the game-changer you’ve been waiting for. Let’s explore how this remarkable tool can transform your wellness journey and why it deserves a spot in your daily routine.
The Importance of Women’s Wellness
Women’s wellness is a vital component of overall health. It encompasses physical, mental, and emotional well-being. Recognizing its significance can lead to improved quality of life.
Women face unique health challenges throughout their lives. From hormonal changes to reproductive health issues, these factors demand attention and care. Prioritizing wellness helps women navigate these complexities with grace.
Mental health deserves equal focus. Stressors from work, family, and societal expectations can take a toll on emotional stability. Engaging in self-care routines fosters resilience.
Additionally, the value of having community support is immense. Connecting with others who share similar experiences creates empowerment and enhances personal growth.
Investing in women’s wellness not only benefits the individual but also enriches families and communities as a whole. A healthier woman contributes positively to society’s fabric while inspiring future generations to prioritize their own well-being.
How GyneCube Works
GyneCube operates through a simple yet innovative design. This silicone support device is crafted to adapt seamlessly to the female anatomy.
Once inserted, it provides gentle but effective pressure on key points, promoting circulation and alleviating discomfort. The soft material ensures comfort during use, making it suitable for daily wear.
The ergonomic shape of GyneCube allows women to engage in their usual activities without hindrance. Whether you’re at work or exercising, GyneCube stays securely in place.
Additionally, this device works with your body’s natural rhythms. Its design encourages better hormonal balance by supporting pelvic health and overall wellness.
Many users report a noticeable difference within weeks of regular use. It becomes an integral part of their self-care routine, enhancing both physical and emotional well-being as they embrace life fully.
Benefits of Using GyneCube
GyneCube offers a range of benefits specifically designed for women’s wellness. Its innovative silicone support provides comfort and stability during various activities, whether at work or while exercising.
Many users report reduced discomfort associated with menstruation and pelvic pressure. The soft yet firm design aligns perfectly with the natural contours of the body, making it an ideal choice for daily use.
Additionally, GyneCube promotes better posture, which can lead to improved overall well-being. With its lightweight and portable nature, it easily fits into any lifestyle whether you’re on a yoga mat or running errands.
Women appreciate how discreetly GyneCube integrates into their routines. This ease of use helps foster a proactive approach to health without sacrificing convenience or style.
Embracing GyneCube enriches the journey toward enhanced physical comfort and empowerment in women’s lives.
Real-Life Success Stories from GyneCube Users
Many women have shared their transformative experiences with GyneCube. One user, Sarah, struggled with menstrual discomfort for years. After incorporating GyneCube into her wellness routine, she noticed a significant reduction in pain and bloating.
Another testimonial comes from Emily, who found that regular use of the silicone support helped regulate her cycle. She felt more balanced and energized throughout the month.
There’s also Amanda’s story she fumbled through postpartum recovery until discovering GyneCube. Its gentle support made her feel more comfortable during a challenging time.
These stories highlight not just relief but empowerment. Women are reclaiming their wellness journeys thanks to this innovative product. Each experience reflects how personalized care can lead to remarkable improvements in daily life and overall health.
Comparison to Other Women’s Wellness Products on the Market
When considering women’s wellness products, GyneCube stands out for its innovative design and targeted support. Unlike many traditional solutions that focus solely on symptom relief, GyneCube promotes overall well-being.
Many competitors rely heavily on pills or supplements, which can lead to unwanted side effects. In contrast, GyneCube’s silicone structure offers a natural approach without the complications of chemical ingredients.
Some products claim comprehensive benefits but lack specific functionality. GyneCube is tailored specifically for women’s needs, ensuring it addresses essential aspects of health effectively.
Price points vary widely among competing brands. However, GyneCube remains competitively priced while delivering unique advantages that justify the investment in one’s health.
Consumer reviews often highlight dissatisfaction with generic options lacking personalization; this is where GyneCube excels by providing customized support based on individual requirements. It truly redefines what women should expect from wellness solutions today.
How to Incorporate GyneCube into Your Daily Routine
Incorporating GyneCube into your daily routine is simple and intuitive. Start by placing it in a visible spot, like your bathroom counter or bedside table. This will serve as a gentle reminder to make it part of your day.
Begin each morning with a quick session while you go about your morning rituals. Whether you’re brushing your teeth or preparing breakfast, take a few moments to use GyneCube for its intended purpose.
You can also set specific times during the day when you feel most stressed or uncomfortable. Pairing its use with relaxation techniques, such as deep breathing or meditation, can enhance its benefits significantly.
Consider integrating GyneCube into wind-down routines at night too; this could help ease tension accumulated throughout the day and promote better sleep quality. The key is consistency make it an effortless addition that flows seamlessly with what you already do every day.
Future Developments and Expansion of the GyneCube Brand
GyneCube is on an exciting path towards growth and innovation. The brand’s commitment to enhancing women’s wellness means that new products are always in the pipeline.
Future developments may explore additional silicone-based solutions tailored for specific health needs, addressing various stages of a woman’s life cycle. Research and feedback from users will drive these innovations, ensuring they resonate with real experiences.
Moreover, GyneCube aims to expand its reach globally. By partnering with healthcare professionals and wellness influencers, the brand hopes to spread awareness about its benefits further.
Educational campaigns could also emerge, focusing on empowering women through knowledge about their bodies and holistic health options. This strategy not only promotes the product but fosters a supportive community around women’s wellness.
With such plans in motion, GyneCube is set to become a pivotal player in reshaping how we think about women’s health products.
Conclusion: Empowering Women’s Health with GyneCube
GyneCube is more than just a product; it’s a commitment to improving women’s health and wellness. With its innovative silicone support design, it offers tangible benefits that can enhance daily life. Many users have shared their positive experiences, highlighting how GyneCube has brought relief during challenging times.
The importance of prioritizing women’s wellness cannot be overstated. With the right tools like GyneCube, women are empowered to take charge of their health journey. As this brand continues to grow and evolve, we can expect even more exciting developments aimed at fostering well-being for all women.
By incorporating GyneCube into your routine, you’re not only investing in yourself but also joining a community dedicated to supporting women’s health on every level. Embrace the change and feel the difference that GyneCube can make in your life today.
HEALTH
Jusziaromntixretos: The Future of Cognitive Training
Introduction to Jusziaromntixretos and Cognitive Training
In a world where cognitive abilities dictate success, the quest for improved mental performance has led to innovative solutions. Enter Jusziaromntixretos a groundbreaking approach to cognitive training that is transforming how individuals enhance their brainpower. As we navigate through an age filled with distractions and information overload, harnessing our cognitive potential becomes essential. This revolutionary method promises not only to sharpen focus but also to elevate overall mental agility. Are you ready to explore this exciting frontier in brain training? Let’s dive into what makes Jusziaromntixretos a game-changer in the realm of cognitive enhancement!
The Science Behind Jusziaromntixretos
Jusziaromntixretos is rooted in cutting-edge cognitive neuroscience. Its approach focuses on enhancing brain plasticity, enabling users to adapt and grow their mental capabilities.
The system employs various techniques such as neurofeedback and gamification. These elements work together to create an engaging environment for users, promoting deeper learning experiences.
Research indicates that targeted cognitive training can improve memory, attention, and problem-solving skills. Jusziaromntixretos harnesses this research by offering tailored exercises designed to stimulate specific areas of the brain.
Additionally, advancements in technology allow real-time tracking of progress. This feedback loop helps individuals understand their strengths and weaknesses more clearly than ever before.
By combining scientific principles with innovative design, Jusziaromntixretos paves a new path in cognitive development. It transforms traditional methods into dynamic experiences that captivate the user’s interest while delivering tangible results.
Benefits of Cognitive Training with Jusziaromntixretos
Cognitive training with jusziaromntixretos offers a wide array of advantages. One significant benefit is enhanced memory retention. Users often report improved recall abilities, which can positively impact daily tasks and learning experiences.
Another advantage lies in increased focus and concentration. Engaging with jusziaromntixretos encourages mental agility, helping individuals maintain attention over extended periods.
Moreover, stress reduction is an unexpected perk. The platform incorporates mindfulness techniques that promote relaxation while stimulating cognitive functions. This dual approach fosters a balanced state of mind.
Social interaction also plays a vital role in the benefits provided by jusziaromntixretos. Many users connect through shared challenges and achievements, creating a supportive community focused on growth.
Regular engagement leads to better problem-solving skills. As users tackle various exercises, they develop innovative strategies for overcoming obstacles in both personal and professional spheres.
How to Get Started with Jusziaromntixretos
Getting started with jusziaromntixretos is easy and straightforward.
First, visit the official website to explore available resources and tools tailored for cognitive training. Registration is usually quick; just fill out a simple form.
Once you’re signed up, dive into the introductory materials. These will guide you through various exercises designed to enhance your cognitive abilities.
Next, set aside dedicated time each day for practice. Consistency is key in developing new skills and improving mental agility.
Connect with other users online or on social media platforms. Sharing experiences can provide motivation and insights that enrich your training journey.
Don’t hesitate to track your progress using built-in analytics features offered by jusziaromntixretos. Monitoring improvements can keep you engaged and focused as you advance in your cognitive training efforts.
Success Stories from Users of Jusziaromntixretos
Many users have shared their transformative experiences with jusziaromntixretos. One individual reported a significant boost in memory recall after just a few weeks of use. Tasks that once felt daunting became manageable.
Another user highlighted improvements in focus and concentration. They noted how they could engage better during meetings, leading to enhanced productivity at work.
Parents often express gratitude for the positive changes they’ve observed in their children’s learning abilities. Kids who struggled with attention now show remarkable enthusiasm for schoolwork.
Athletes are also reaping benefits, citing sharper decision-making skills during high-pressure situations. This cognitive edge can make all the difference in competitive environments.
Each story adds to the growing testament of jusziaromntixretos’ impact on daily life and performance across various domains.
Potential Future Developments for Jusziaromntixretos
As the landscape of cognitive training evolves, so does jusziaromntixretos. The future may see enhanced personalization features. Users could benefit from tailored programs that adapt to their specific needs and preferences.
Integrating artificial intelligence might open new avenues for deeper insights into user performance. Predictive analytics could offer suggestions based on individual progress patterns.
Gamification is another exciting frontier. By incorporating game-like elements, learning becomes more engaging and enjoyable, encouraging consistent use among participants.
Moreover, expanding access through mobile applications would allow users to train anytime and anywhere. This adaptability may encourage more people to get involved.
Collaborations with educational institutions or wellness programs might also emerge, bridging cognitive training with broader health initiatives for a holistic approach to mental well-being.
Conclusion
Cognitive training is evolving rapidly, and the introduction of jusziaromntixretos marks a significant milestone in this journey. As more people become aware of its potential, it’s clear that integrating this innovative approach into daily routines can lead to profound benefits. From enhancing memory to boosting cognitive agility, the possibilities are expansive.
As we look ahead, the future seems bright for jusziaromntixretos and those who embrace its power. With ongoing research and development, new features and applications will surely emerge. For anyone interested in maximizing their mental capacity or simply looking for a way to stay sharp as they age, exploring jusziaromntixretos could be a game-changer.
Getting started is easy; all it takes is curiosity and a willingness to engage with your mind on a deeper level. The success stories pouring in from users highlight just how transformative this experience can be. By joining the community around jusziaromntixretos today, you take an exciting step toward unlocking your brain’s full potential.
The path forward is filled with promise both for individuals seeking improvement and researchers excited about what comes next. The world of cognitive training continues to expand, inviting everyone along for the ride into uncharted territories of human capability.

 HOME IMPROVEMENT11 months ago
HOME IMPROVEMENT11 months agoThe Do’s and Don’ts of Renting Rubbish Bins for Your Next Renovation

 BUSINESS12 months ago
BUSINESS12 months agoExploring the Benefits of Commercial Printing

 BUSINESS11 months ago
BUSINESS11 months agoBrand Visibility with Imprint Now and Custom Poly Mailers

 TECHNOLOGY10 months ago
TECHNOLOGY10 months agoDizipal 608: The Tech Revolution Redefined

 HEALTH7 months ago
HEALTH7 months agoThe Surprising Benefits of Weight Loss Peptides You Need to Know

 HEALTH7 months ago
HEALTH7 months agoYour Guide to Shedding Pounds in the Digital Age

 HEALTH10 months ago
HEALTH10 months agoHappy Hippo Kratom Reviews: Read Before You Buy!

 HOME IMPROVEMENT7 months ago
HOME IMPROVEMENT7 months agoGet Your Grout to Gleam With These Easy-To-Follow Tips












