Intraoral cameras have revolutionized dental care by enhancing communication between dentists and patients. Understanding the key features of these devices can significantly impact diagnostic accuracy and treatment planning. This article explores the essential features to consider when choosing an intraoral camera, ensuring dental professionals can provide the best possible care.
Overview of Intraoral Cameras
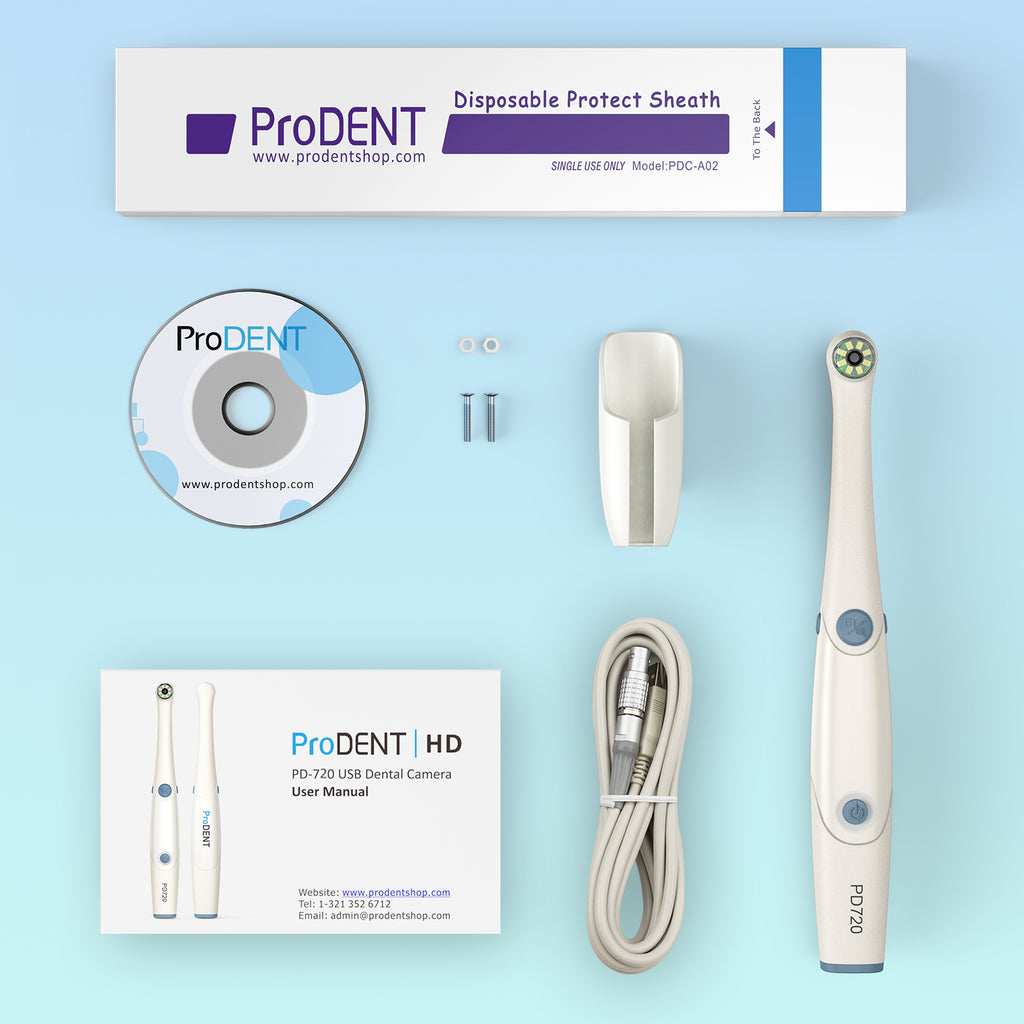
Intraoral camera is essential tools in modern dentistry. Intraoral cameras allow dentists to capture high-resolution images of a patient’s mouth, facilitating better visualization of dental issues. The primary features of intraoral cameras greatly impact their functionality and effectiveness.
Image Quality
Image quality is crucial when selecting an intraoral camera. High-definition cameras provide clear, detailed images, enabling effective diagnosis. Look for cameras that offer at least 720p resolution, as this standard often results in enhanced clarity and precision.
Lighting Options
Intraoral cameras should incorporate adequate lighting solutions. Bright LED lights improve visibility, helping to highlight issues that might be difficult to see with traditional lighting. Adjustable brightness settings add versatility, allowing customization for different clinical situations.
Size and Design
The design and size of the intraoral camera affect usability. Compact cameras are easier to maneuver in a patient’s mouth while offering comfort. Ergonomic designs enable dentists to capture images without causing discomfort, promoting patient cooperation during examinations.
Connectivity
Connectivity features are vital for seamless integration into dental practice. Many intraoral cameras support USB and wireless connections, allowing easy transfer of images to computers and practice management software. This feature simplifies data documentation and enhances communication with patients.
Software Compatibility
Software compatibility is essential for effective image management. Intraoral cameras should be compatible with various software platforms used for patient records. This ensures efficient sharing of images and supports treatment planning discussions between dentists and patients.
Durability and Hygiene
Durability ensures longevity, making it an important consideration. Intraoral cameras should withstand regular use and cleaning. Waterproof and easy-to-disinfect materials are preferred, enhancing hygiene and adhering to infection control protocols.
Cost-Effectiveness
Cost plays a significant role in decision-making for dental practices. While higher-priced options may offer advanced features, it’s essential to evaluate the return on investment. Assess the combination of features and quality that suit the practice’s specific needs and budget.
Intraoral cameras significantly aid in diagnosis and patient communication. Understanding these key features assists dental professionals in selecting the right device for their practice, ultimately improving patient care and treatment outcomes.
Image Quality
Image quality stands as a crucial factor when selecting an intraoral camera. High-resolution images improve diagnostic capabilities and facilitate effective communication with patients.
Resolution
Resolution refers to the amount of detail an image holds. Intraoral cameras should offer at least 1.3 megapixels, ensuring clarity for small dental nuances. Higher megapixel counts, such as 2 megapixels or more, provide sharper images, enabling better visualization of cavities, cracks, and other dental issues. Excellent resolution assists dentists in making informed decisions regarding treatment options.
Frame Rate
Frame rate measures how many frames are captured per second. A frame rate of 30 frames per second (fps) or higher enhances video quality, particularly during real-time examinations or patient demonstrations. Higher frame rates also reduce motion blur, providing clearer images during dynamic operations like tooth examinations. This ensures that dentists can observe subtle movements and changes, contributing to more accurate assessments.
Ease of Use
Ease of use is essential for maximizing the effectiveness of an intraoral camera. Features that improve usability improve workflows and patient care.
Ergonomic Design
An ergonomic design ensures that the intraoral camera fits comfortably in the dental professional’s hand. Lightweight models reduce fatigue during extended use. A streamlined shape allows easy maneuverability within the oral cavity, enabling better access to hard-to-reach areas. This design aspect enhances precision in capturing images and providing accurate diagnoses.
User Interface
A user-friendly interface promotes efficiency during dental procedures. Intuitive controls allow for quick adjustments to settings, such as zoom and focus. Clear icons and responsive touchscreens facilitate seamless navigation. When evaluating intraoral cameras, it’s important to consider models with customizable settings that cater to specific practice needs, enhancing the overall experience for both the clinician and the patient.
Connectivity Options
Connectivity options play a crucial role in the functionality of intraoral cameras. These features determine how easily the camera integrates with a dental practice’s existing infrastructure, enhancing workflow and data management.
USB Connectivity
USB connectivity offers a straightforward way to transfer high-quality images and videos from the intraoral camera to computers or other devices. Cameras with USB connections typically use USB 2.0 or USB 3.0 ports, ensuring fast data transfer rates. Selecting a model that supports plug-and-play functionality simplifies setup, allowing for immediate use without complicated installation processes. Additionally, USB connectivity allows for easy updates and maintenance of camera software, helping maintain the relevance of the device over time.
Wireless Capability
Wireless capability provides enhanced flexibility and mobility during dental procedures. Intraoral cameras with Wi-Fi or Bluetooth connectivity eliminate the need for cables, allowing dental professionals to move freely while capturing images. This wireless feature facilitates seamless integration with practice management software, enabling immediate access to patient records and image storage. Additionally, wireless cameras are often compact and rechargeable, further increasing their usability in a busy dental setting. It’s essential to ensure that the wireless connection remains stable and secure to prevent data loss during image transmission.
Durability and Maintenance
Durability and ease of maintenance are critical factors when selecting an intraoral camera. These elements directly affect the device’s lifespan and performance in a dental practice.
Build Quality
Build quality refers to the materials and construction of the intraoral camera. A robust design ensures the camera can withstand daily use and potential drops. Stainless steel or high-grade plastic components provide durability while resisting wear and tear. Cameras with reinforced casings often endure harsher conditions, making them suitable for busy dental environments. Additionally, weight and balance in the design contribute to user comfort, allowing dental professionals to operate the device without strain.
Cleaning and Sterilization
Cleaning and sterilization processes are essential for maintaining hygiene in dental settings. Intraoral cameras should allow for easy access to all surfaces, facilitating thorough cleaning. Look for models that are compatible with standard disinfectants and have removable components for deep cleaning. Autoclavable options improve safety by ensuring that all parts can undergo sterilization. Proper maintenance practices, such as routine inspections and adherence to manufacturer guidelines, help ensure the camera remains in top working condition, prolonging its operational life.
Cost and Value
Cost and value play significant roles in selecting an intraoral camera. Understanding these factors helps dental professionals make informed choices that align with their practice needs.
Budget Options
Budget options for intraoral cameras range from $200 to $1,000. These cameras often include essential features, such as basic image quality and straightforward connectivity, making them suitable for smaller practices or those just starting. While these models may lack advanced functionalities, they still provide adequate performance for routine examinations and patient education.
Investment Considerations
Investment considerations include long-term costs and potential savings. Higher-end models, priced between $3,00 and $10,00, offer superior image quality, enhanced durability, and advanced features. Such cameras often lead to improved diagnostic accuracy and better patient communication, resulting in increased treatment acceptance. Evaluating warranty options also extends the camera’s value by protecting against costly repairs. Choosing a reliable camera minimizes replacement needs, ensuring that the initial investment pays off over time.
Conclusion
Selecting the right intraoral camera is vital for enhancing patient care and diagnostic accuracy. By focusing on key features like image quality, ergonomic design, and connectivity options, dental professionals can make informed decisions that align with their practice needs. Durability and ease of maintenance also play crucial roles in ensuring the longevity of these devices.
Investing in a quality intraoral camera not only improves communication with patients but also streamlines workflows within the practice. Ultimately, understanding these essential features can lead to better treatment outcomes and a more efficient dental practice.